Radically Resilient Health Podcast
THE GUT BRAIN CONNECTION: PART 1 – DIGESTION
WHAT IS THE CONNECTION?
PHYSIOLOGICAL FRIENDS OR FRENEMIES?
Written By Leah GiaQuinta, PT and Dr Carolyn Dolan, DPT, MSHN
The gut-brain connection is not a new concept. We talk about this relationship frequently in our daily conversations. Often when our brains process emotions, we mention those feelings as they relate to our guts. Worried? “I’m sick to my stomach!” Traumatized? “That’s gut-wrenching!” Intuitive? “I have a gut feeling…” Brave? “She’s got guts!” It is nearly impossible to discuss wellness and nutrition without establishing a good understanding of the connection between the gut and the brain. Depending on the status of this interconnected relationship, the two can function as physiological friends or “frenemies.” Here we can break down how this relationship is important to the overall healing and well-being of our bodies.
The science
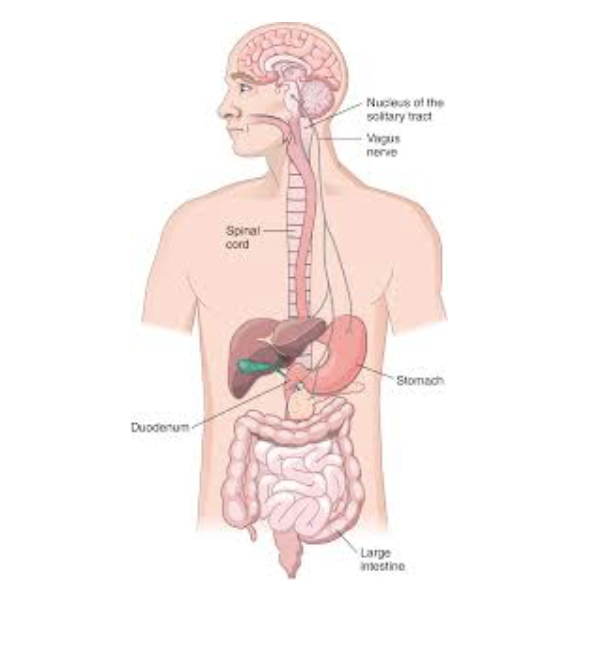
Fundamental anatomy shows us that the gut and the brain are physically connected. The Vagus Nerve is a cranial nerve from our central nervous system that stretches from our brains to our stomachs and intestines. Not only does our brain send signals to our gut, but our gut sends signals back to our brain. This is called a feedback loop. The feedback loop will create a cause-and-effect dynamic between one organ and the other. The obvious signals that we might consider in this cause-effect scenario could include hunger / satiety scenarios. An empty stomach may send a signal, “I’m hungry!” up to our brains, which prompts us to get up and eat. In a healthy system, both organs will have a positive effect on the other in this cycle of communication. But what happens if one or both organs are stressed, impaired or inflamed?
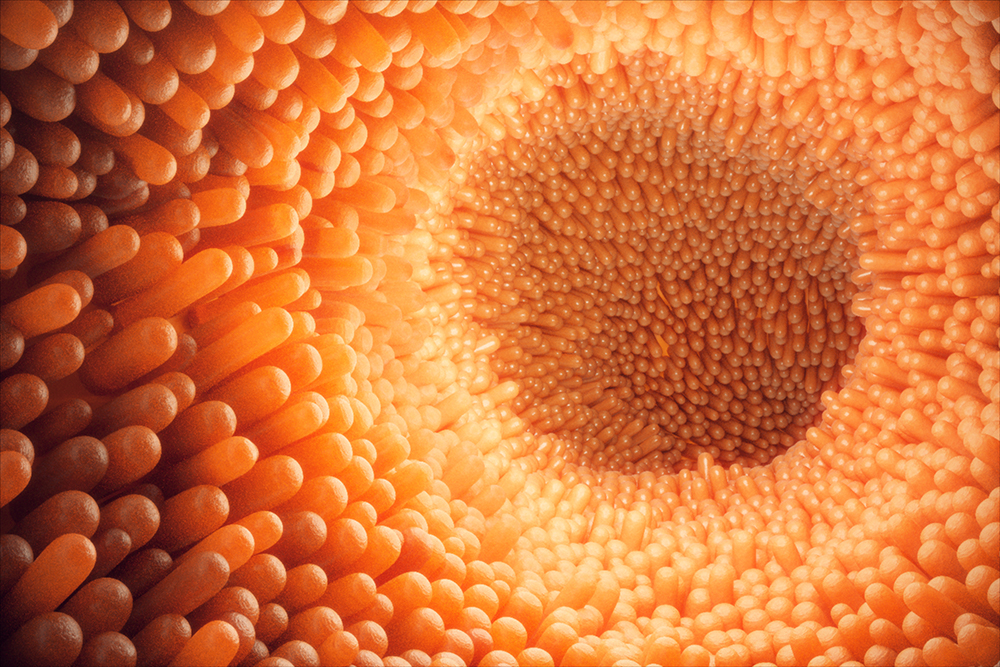
When our brains are inflamed or overactive, consequential effects may occur in our guts. Many animal studies have observed subjects with central nervous system injuries like traumatic brain injuries have identified this connection. In these studies, mechanical destruction that occurred in the brain revealed disruptions in the feedback loop with the gut. Results found subjects with weakenings in the tight junctions within their intestinal linings. This is called intestinal permeability, or “leaky gut.” When this occurs, the gut lining can no longer serve as a barrier to protect our bodies. Without a protective barrier, our bodies may experience systemic inflammation because nutrients are not able to optimally absorb into this lining and into our bodies. Moreover, various food particles may pass through the weakened junctions of our gut lining into areas where they don’t belong. The more that we can decrease the overall inflammation of the brain and its system, the more we can allow our bodies to heal by promoting a healthy gut environment.
“Researchers have known for some time now that the cornerstone of all degenerative conditions, including brain disorders, is inflammation.” – David Perlmutter, MD, Grain Brain
Conversely, If our guts are unhealthy, we may experience adverse effects on our brains. Our brains interpret how we perceive pain and how we behave. If a disruption occurs in this loop by consuming foods that can compromise our gut lining, the result often leads to systemic inflammation. For example, diets that include excessive amounts of gluten, refined sugars, antibiotics or some pharmaceuticals have been shown to have compromising effects on gut health. Here, a compromised gut lining can lead to systemic inflammation which weakens the brain barrier. The effect of a compromised gut-brain connection may result in exacerbated neurologic symptoms like anxiety, depression or other inflammatory brain disorders. Our brains regulate more than our moods; our brains also are an important component in our sensory systems as they relate to pain. If a compromised gut leads to an exacerbation of our perceptions of pain, we may experience increased intensities and/ or durations of pain symptoms.
For this reason, when we experience an injury localized to an adjacent area in our bodies, a whole-picture approach including the gut-brain connection and our nutritional behaviors may offer a component piece that can positively or negatively affect injury recovery. We will continue to take a closer look at how this relates to localized vs. systemic inflammation, but it is important to recognize that by promoting nutrient absorption within a healthy gut, we can promote a normalized healing response within our whole system. The first step is to acknowledge the gut-brain connection and to optimize it. Then will we be able to create desired outcomes of healing and wellness by building radical resilience within our whole bodies.
No guts…no glory!
___________________________________________________________
References:
- Central Nervous System injury and intestinal permeability
- Dietary influences on intestinal permeability
Mena
Radically Resilient Health Podcast Small Steps Conquer Mountains with Special Guest Mena Spodobalski Evoke Fitness owner, Mena Spodobalski, shares her joys and struggles toward radically resilient health. Health doesn't always have to seem radical. The best workout...
Recovery From Substance Dependency With Lori Windfelt
Radically Resilient Health Podcast Recovery From Substance Dependency With Lori Windfelt Radically Resilient Health is not about the absence of disease, injury, or stress, it is the ability to recover and make positive choices to support your overall health. Lori...
Emotional and Mental Resiliency – With Special Guest Dusty Braun
Radically Resilient Health Podcast Emotional and Mental Resiliency With Dr. Dusty Braun Our mind and body are intimately interconnected in ways that we can't really comprehend outside of science. We oftentimes think ourselves or our minds as separate from our body,...
Available at our partner locations

690 West 2nd St. Suite 101
Reno, NV 89503

13981 S Virginia St #402b,
Reno, NV 89511